Research and Resources
Explore resources on gut-brain health, hormones, inflammation, autoimmune disorders and the effect on mental wellness.

More to the Story
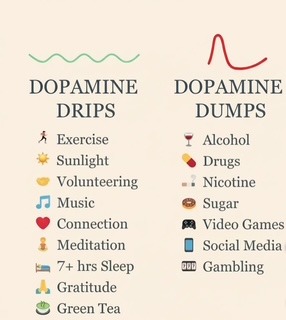
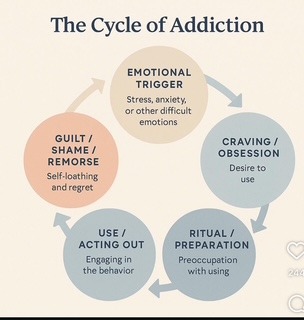
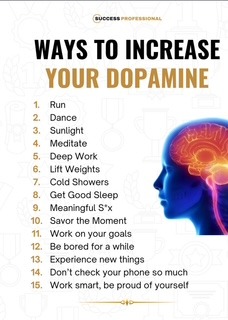
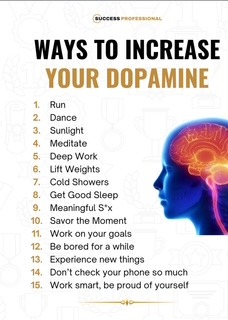
Dopamine
Dopamine drives motivation, reward, and feelings of pleasure, but modern society constantly overstimulates this system through social media, instant notifications, processed foods, online shopping, and other “quick-hit” rewards. These repeated dopamine spikes make the brain crave fast gratification, increasing vulnerability to addiction while dulling the ability to enjoy normal, everyday experiences. Over time, this can lower baseline dopamine functioning, contributing to depression, low motivation, and emotional numbness.





Explore innovative testing and treatment options for gut-brain connection and lifestyle changes.
Gut-Brain Axis
Stool testing (microbiome analysis): Looks at the balance of gut bacteria, yeast, and other microbes. Can identify overgrowths or missing strains linked to inflammation or mood.
Bloodwork: Includes markers for thyroid, hormones, vitamin levels (like B12, D, folate), and inflammation (CRP, cytokines). These can affect both gut and brain health.
Food sensitivity testing: Helps identify foods that may be triggering gut inflammation and symptoms.
Functional lab panels: May check for gut permeability (“leaky gut”), adrenal function, or nutrient absorption issues.
Treatment Options
Nutrition: Eating more fiber, fermented foods, and plant-based diversity supports a healthy microbiome.
Probiotics & prebiotics: Supplements or foods that add healthy bacteria or feed them. Evidence shows some strains may reduce anxiety and depression.
Lifestyle: Stress management, exercise, and good sleep improve both gut balance and brain resilience.
Medication & integrative care: Antidepressants, anti-anxiety medication, or hormone support may be combined with nutrition and lifestyle changes for a whole-person approach.
Targeted support: In some cases, doctors may recommend anti-inflammatory supplements (like omega-3s), gut repair nutrients (like zinc or L-glutamine), or tailored probiotic strains.
Inflammation
hs-CRP (high sensitivity C-reactive protein): sensitive marker for chronic low-grade inflammation, linked to depression and cardiovascular risk.
ESR (erythrocyte sedimentation rate): shows systemic inflammation, though less specific.
Ferritin: elevated in chronic inflammation or infection (also iron status marker).
Fibrinogen: clotting protein that rises with inflammation.
Homocysteine: high levels indicate oxidative stress and vascular inflammation.
Cytokine & Immune Signaling Panels (specialty labs)
IL-6 (interleukin-6): strongly linked with depression, fatigue, and chronic illness.
TNF-α (tumor necrosis factor alpha): pro-inflammatory cytokine associated with mood changes and neuroinflammation.
IL-1β: another key cytokine in “sickness behavior” (fatigue, low motivation).
IL-10: anti-inflammatory cytokine; low levels may suggest poor immune regulation.
IFN-γ (interferon gamma): immune activation marker, sometimes elevated in viral triggers.
Oxidative Stress & Cell Damage
8-OHdG (8-hydroxy-2’-deoxyguanosine): marker of oxidative DNA damage.
Malondialdehyde (MDA): lipid peroxidation marker.
Glutathione (reduced/oxidized ratio): body’s main antioxidant buffer.
Metabolic & Vascular Inflammation
Adiponectin & leptin: imbalances linked to insulin resistance and inflammation.
Lp-PLA2 (lipoprotein-associated phospholipase A2): vascular inflammation marker.
GlycA (Glycoprotein acetylation): advanced marker of systemic inflammation used in research/clinical labs.
Gut-Immune Markers
Calprotectin, Lactoferrin: stool markers of gut inflammation.
Zonulin: marker of gut permeability (“leaky gut”).
sIgA (secretory IgA): mucosal immunity indicator.
Short-chain fatty acids (butyrate, acetate, propionate): beneficial anti-inflammatory metabolites (low levels suggest dysbiosis).
Autoimmune screens
ANA (antinuclear antibody)
Rheumatoid factor, anti-CCP
Thyroid antibodies (TPO, TgAb)
HLA typing if autoimmune suspicion (celiac, ankylosing spondylitis)
Other disease-specific antibodies (SSA/SSB, dsDNA, etc. as indicated)
Viral / infectious panels
EBV (Epstein–Barr virus) antibodies (IgG, IgM) – linked to fatigue and chronic activation
CMV (Cytomegalovirus) antibodies
Lyme and co-infections (Borrelia, Babesia, Bartonella – region dependent)
HHV-6 (human herpesvirus 6) titers
Hepatitis panel (if risk factors present)
HIV screen (standard of care in unexplained immune issues)
Hormonal Balance
Testing
Bloodwork: Measures thyroid hormones, estrogen, progesterone, testosterone, and cortisol to check for imbalances.
Saliva or urine hormone panels: Sometimes used to track daily hormone fluctuations or adrenal function.
Vitamin and nutrient testing: Low levels of B12, D, folate, or iron can mimic or worsen mood problems.
Functional testing: In some cases, providers may check for inflammation markers or gut health, since these interact with hormones.
Treatment
Lifestyle support: Stress management, exercise, and healthy sleep patterns naturally improve hormone balance.
Nutrition: Balanced meals with enough protein, healthy fats, and micronutrients support hormone production.
Medications: Antidepressants, thyroid medication, or other psychiatric/medical treatments may be needed.
Hormone therapy: Options like thyroid replacement, testosterone therapy for men, or estrogen/progesterone support for women can restore balance when levels are low.
Integrative care: Supplements (omega-3s, vitamin D, adaptogens, etc.) may be added, guided by lab results and medical advice.
Contact Information
Secure Text Message: 203-594-6554
email: Sharonf@sharonfarahcare.com
Accepting Insurance: Husky, Anthem, Aetna and Cigna
If you don’t see a time that works, feel free to send us a secure text message for additional appointment options, special requests, or any questions. We’re always happy to help.
Manage appointments, records, labs, medications, and billing securely in one Patient Portal.
Click button below to access patient portal
